A new group of healthcare providers hopes to address the high rate of colon cancer deaths among Black Americans with a national push to increase screening levels.
Organized by Stand Up To Cancer, the Colorectal Cancer Health Equity Dream Team is specifically looking at screening in underserved areas where Blacks have notched higher incidence of colon cancer and related deaths than other ethnic groups.
Each year, the disease claims more than 50,000 lives in the United States as the third-most common form of cancer and second-most common cause of cancer-related death. In the Black community, numbers are even higher, largely due to less screening, a diagnostic tool connected to early detection and higher survival rates.
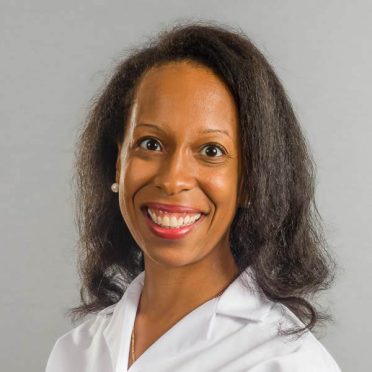
Not only are African Americans more apt to get colon cancer, but they also are diagnosed more at younger ages and when the disease is advanced, said Dr. Chioma Anjou, a gastroenterology specialist with Hartford HealthCare’s Digestive Health Center.
“We consider both environmental and genetic contributions,” Dr. Anjou said. “No specific gene giving African Americans higher rates of colon cancer has been identified. There are some hypotheses and associations, but no single causative gene that we can point to that are responsible for the worse outcomes among African-Americans.”
One possibility is that African Americans may present more with sessile serrated adenoma, a type of polyp that is flatter and harder to see during colonoscopy.
“There is also some evidence that the response to treatment typically used for stage 2 and 3 colon cancers is lower in African Americans,” Dr. Anjou said.
Environmental factors impacting rates in African Americans include:
- Being less likely to talk with family about history of colon polyps.
- Discomfort talking about symptoms.
- Inability to share screening results with relatives, even if colon polyps are found.
Systemic health disparities also play a role, Dr. Anjou said. A recent publication determined the length of time between colon cancer diagnosis and treatment was longer for minorities, improving from lower to higher socioeconomic status except among African Americans. Even for high-income African Americans, the research, published in Gastroenterology, showed longer times between diagnosis and treatment.
“Why does this matter? Aside from the obvious reasons, data shows that for a delay of 30 days in treatment, the risk of dying increases by one-and-a half times,” Dr. Anjou said, citing another study.
While the Stand Up To Cancer team works in three areas across the country, including Greater Boston, there are things everyone can do to change this deadly trend.
Dr, Anjou urged people of all races to:
- Follow federal guidelines for screening. Currently, anyone over the age of 45 should have a colonoscopy to check for signs of colon cancer.
- Find out your family history of this and other diseases.
- Bring any symptoms to your primary care doctor. Symptoms include rectal bleeding, unexpected weight loss, changes in bowel patterns or abdominal discomfort.
- Spread the word about the importance of screening.