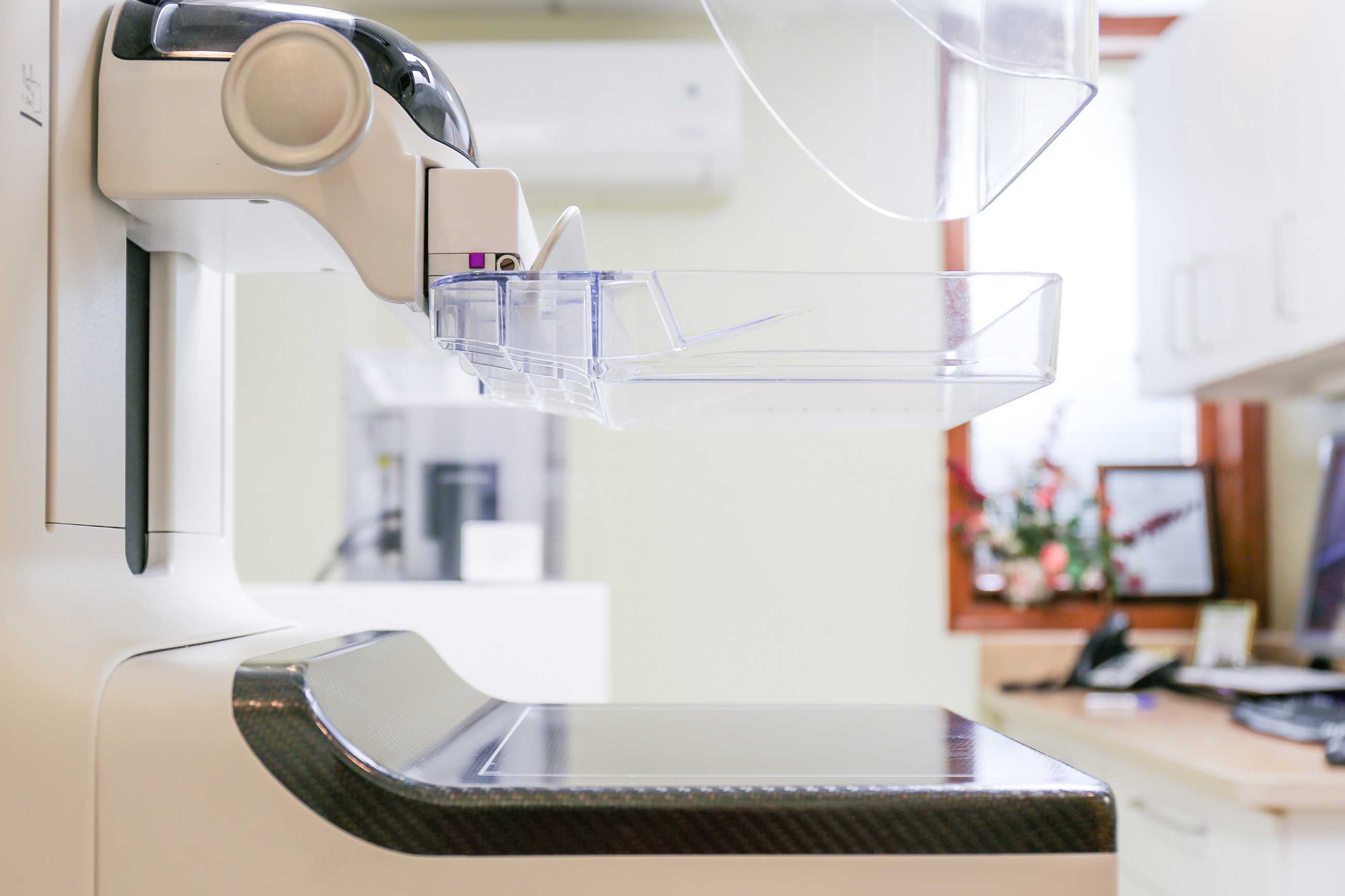
MidState Medical Center and The Hospital of Central Connecticut (HOCC) are the latest Hartford HealthCare organizations to add the leading-edge 3D mammography technology.
For patients and providers, 3D mammography can provide clearer views of suspicious masses, improve diagnosis and reduce unnecessary testing.
Although 3D mammography has been around for years, the technology has continued to evolve. MidState, HOCC, Backus Hospital, Hartford Hospital and Windham Hospital have all implemented this latest version of 3D mammography — also known as breast tomosynthesis.
During a 3D mammography scan, the X-ray arm sweeps over the breast to take multiple images. Unlike traditional 2D technology in which the mammography is read as a single image, 3D imaging allows the radiologist to scroll through the images like the pages of a book and view through overlapping tissue.
Overlapping tissue is a common problem for women with dense breasts, leading to call-backs in more than 10-percent of cases, according to Backus radiologist Stacy Spooner, MD.
“For women with dense breasts, which is a significant portion of our population, tomosynthesis allows us to find masses and other areas of concern that we might not see in traditional 2D mammography,” says Dr. Spooner.
Holley Dey, MD, Chief of Mammography and Women’s Health at MidState, said studies show a 40% increase in the ability to diagnose invasive cancer and a 28 % reduction in unnecessary tests.
Breast cancer is the top diagnosed cancer across Hartford HealthCare. In 2016, there were over 1,200 breast cancers diagnosed here. In Connecticut, we have a high rate of compliance with mammography screening, and early detection leads to better outcomes. According breastcancer.org:
- About 1 in 8 U.S. women (about 12.4%) will develop invasive breast cancer over the course of her lifetime.
- In 2018, an estimated 266,120 new cases of invasive breast cancer are expected to be diagnosed in women in the U.S., along with 63,960 new cases of non-invasive (in situ) breast cancer.
- About 2,550 new cases of invasive breast cancer are expected to be diagnosed in men in 2018. A man’s lifetime risk of breast cancer is about 1 in 1,000.
- Besides skin cancer, breast cancer is the most commonly diagnosed cancer among American women. In 2017, it’s estimated that about 30% of newly diagnosed cancers in women will be breast cancers.
- In women under 45, breast cancer is more common in African-American women than white women. Overall, African-American women are more likely to die of breast cancer. For Asian, Hispanic, and Native-American women, the risk of developing and dying from breast cancer is lower.
- As of January 2018, there are more than 3.1 million women with a history of breast cancer in the U.S. This includes women currently being treated and women who have finished treatment.
- About 5-10% of breast cancers can be linked to gene mutations (abnormal changes) inherited from one’s mother or father. Mutations of the BRCA1 and BRCA2 genes are the most common. On average, women with a BRCA1 mutation have a 55-65% lifetime risk of developing breast cancer. For women with a BRCA2 mutation, the risk is 45%. Breast cancer that is positive for the BRCA1 or BRCA2 mutations tends to develop more often in younger women. An increased ovarian cancer risk is also associated with these genetic mutations. In men, BRCA2 mutations are associated with a lifetime breast cancer risk of about 6.8%; BRCA1 mutations are a less frequent cause of breast cancer in men.
- About 85% of breast cancers occur in women who have no family history of breast cancer. These occur due to genetic mutations that happen as a result of the aging process and life in general, rather than inherited mutations.
- The most significant risk factors for breast cancer are gender (being a woman) and age (growing older).
For more information on imaging services at MidState Medical Center, click here. For more information on imaging services at the Hospital of Central Connecticut, click here.