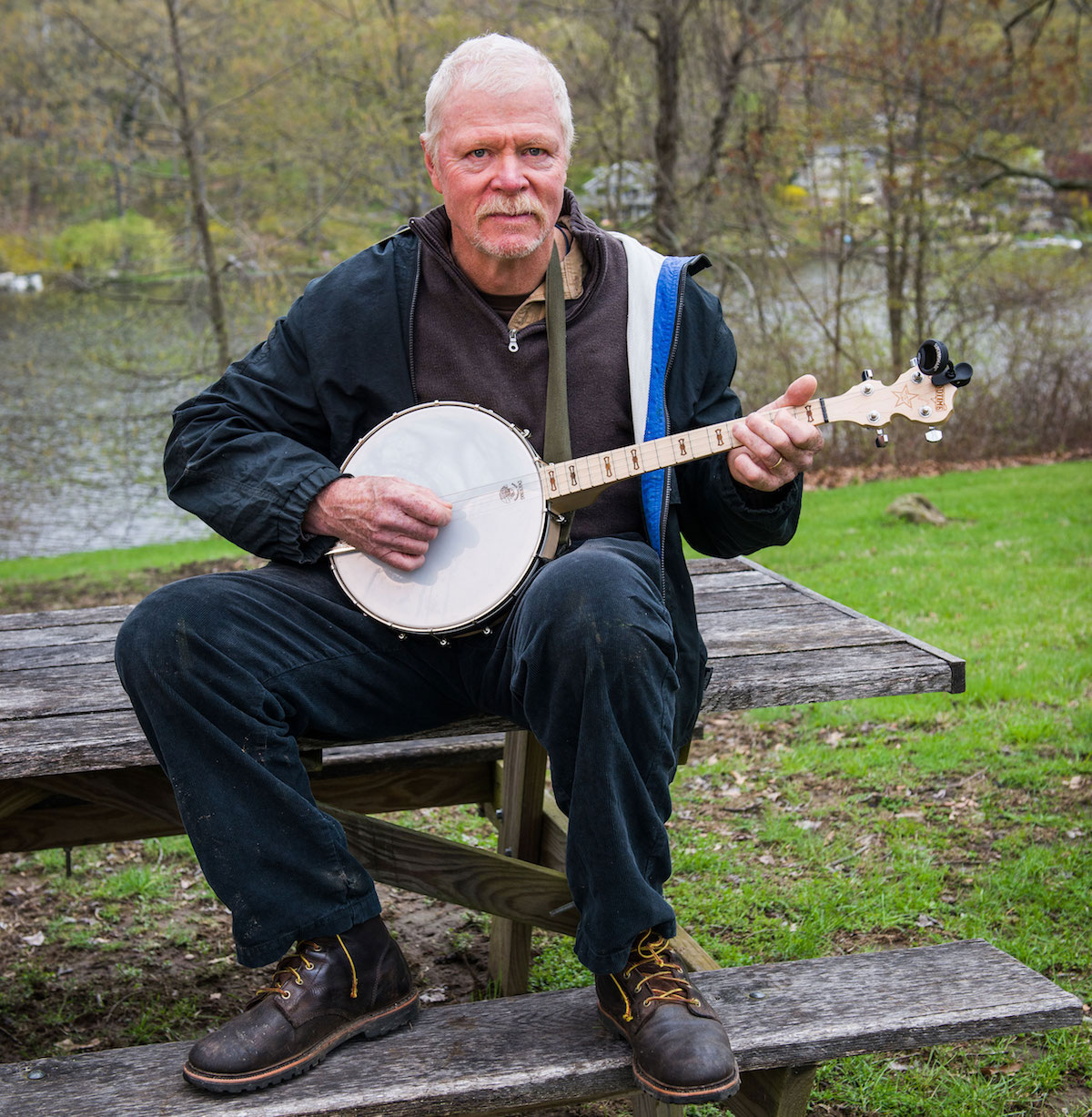
Paul Cochrane hadn’t picked up his banjo in years, ever since Parkinson’s disease had caused tremors that prevented his fingers from plucking the strings to any semblance of a tune.
But, after having the Vercise Gevia Deep Brain Stimulation (DBS) battery implanted in January and turned and adjusted over the following weeks, he has regained control of his muscles and his fine motor skills have improved enough that he can make music again.
“I saw some immediate response. It cuts out the valleys when the medication starts to wear off,” the 62-year-old Patterson, N.Y., resident said. “I have much better fine motor control now.”
The Chase Family Movement Disorders Center at the Hartford HealthCare Ayer Neuroscience Institute was the first facility in the Northeast and among the first nationwide to implant the advanced battery, newly approved by the Food and Drug Administration, to treat the symptoms of Parkinson’s. Neurosurgeon Dr. Patrick Senatus implanted the battery in Cochrane, a patient of Dr. Michelle Lavallee Dagostine, a neurologist.
“We are committed to offering the people in our community the most advanced medical technologies and, in this case, that was the new Vercise System,” said Dr. Senatus, director of the DBS Program for the Ayer Neuroscience Institute. “The technology will help people like Mr. Cochrane with symptoms of this debilitating disease.”
DBS works by stimulating a targeted region of the brain through implanted leads that are powered by a device called an implantable pulse generator. Unlike other DBS systems which are built from pacemaker technology, the Vercise DBS System taps cochlear implant technology and the way it precisely stimulates auditory nerves to replicate hearing.
“This system can adapt therapy to address fluctuations in an individual patient’s symptoms and the progressive nature of Parkinson’s. This allows us to program the device specifically to each patient’s needs and more precisely target their symptoms,” Dr. Senatus explained.
Cochrane opted for surgery after 10 years on medication for his Parkinson’s.
“The last two years, it was getting really bad,” said the retired respiratory therapist who opted for a medication pump last year that would deliver his medication directly into his stomach. Instead of benefitting from the faster delivery, got ulcers instead and had to stop using the pump.
Such a medication history is not unusual for patients with Parkinson’s, many of whom suffer from tremors, muscle rigidity, postural instability and slowed movement. Five years after diagnosis, the average Parkinson’s patient takes medication four times a day and has changed their medication regimen three times.
“Our goal is to improve their quality of life, and we believe deep brain stimulation is an effective way to do that,” Dr. Senatus said.
During surgery, he implants the pulse generator under the skin on the patient’s chest or abdomen and leads trace from there to the targeted part of the brain. When the system is turned on, a remote is used to send a pre-determined program of mild electrical impulses to stimulate the brain.
The new system is the smallest ever made and has a battery life of 15 years or more. Studies in Europe, where Vercise has been approved for use since 2012, and the United States showed the device yielded good control of Parkinson’s symptoms, including a 63-percent improvement in motor function.
For more information on the Deep Brain Stimulation Program at Hartford HealthCare, click here.