By Dr. Chike Chukwumah
How common are hernias? Surgeons at the Hernia Center at Hartford Hospital repair more than 1,000 every year. Nationally, more than 1 million hernias are repaired each year, according to the Food & Drug Administration.
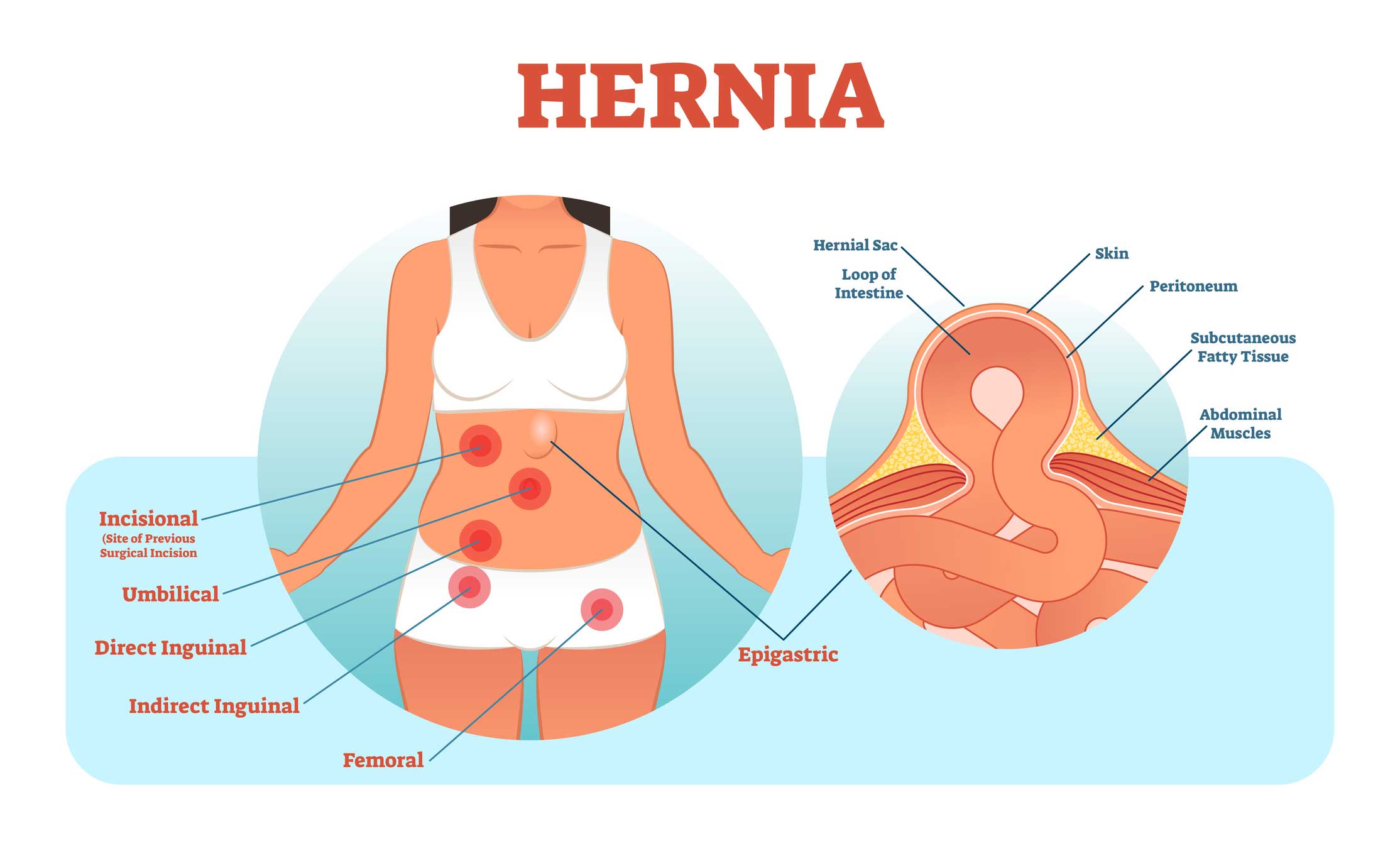
When you get one, you’ll usually know it: an organ or tissue bulges through an abnormal opening, often an intestine (or some portion of the intestine) through a weakened abdominal wall.
Here’s what you should know about hernias:
Q. What are the symptoms of a hernia?
A. The most common symptoms are a bulge or lump, with or without pain. However, many people with a hernia suffer from no symptoms at all initially. Other symptoms include nausea, vomiting or even constipation or an inability to empty the bladder. Because the signs are not always obvious and can mimic other conditions, if you have any of these signs and suspect you may have a hernia, you should call your doctor for an examination.
Q. What are the different types of hernias?
A. There are several types, but inguinal hernias are by far the most common.
An inguinal hernia refers to a hernia in the groin — the area where the abdomen and the thighs connect. Inguinal hernias account for about 80 percent of all hernias, and they are much more common in men than women. However, women can also experience them.
Another type of hernia is a femoral hernia. Femoral canals are channels between the abdomen and thighs where blood vessels and nerves pass. Any bulge is usually in the upper part of the affected thigh just below the groin. Femoral hernias account for about 4 percent of groin-area hernias, but are much more common in women than in men.
Ventral hernias are a protrusion through a weakness in the muscles that form the (anterior) abdominal wall. Ventral hernias present with the same symptoms and risks as other hernias.
Finally, the most common ventral hernias are umbilical hernias, which are associated with a weakness at the umbilicus — more commonly known as the naval. In the womb, it is normal for some of a fetus’ intestines to be located in a sac within the umbilical cord outside the abdomen — the abdominal cavity doesn’t develop at the same rate as the intestines. By birth, the intestines normally have returned to the abdomen and the opening is closed up. If the closure is defective, an umbilical hernia can result, either at birth or as a result of weakening later in life.
Q. How does someone get a hernia?
A. Some people develop a hernia spontaneously, and others may be predisposed. It’s thought that people who are predisposed may have an issue with collagen and how it responds to tension. Other times, a hernia may occur after a trauma like a surgical incision or fall.
Q. Who is at risk for a hernia?
A. Men are more at risk because they typically do more strenuous activities. A major risk factor is persistent abdominal pressure, which can result from morbid obesity. Surgical incisions can also pose a risk, although genetic predisposition plays a key role here. However, even in predisposed people, for instance, if you took 100 people and did the same surgery on them, some would develop a hernia and others would not.
Q. How will a doctor know I have a hernia?
A. If you think you may have a hernia, see your doctor for a physical exam and a review of your history. Your doctor may also recommend an imaging test like an ultrasound or CT scan to confirm a hernia diagnosis.
Q. How long does it take to recover from hernia surgery?
A. When hernia surgery is straightforward, the surgery is done on an outpatient basis, meaning you go home the same day. You can expect your recovery to be from 1 to 3 weeks. If your surgery is more complex, you may need inpatient surgery, which means you will stay overnight or several days in the hospital. In this case, your recovery would be a bit longer, anywhere from 3 to 6 weeks.
Q. What are the restrictions during recovery?
A. The restrictions you have during your recovery are based on your personal and professional lifestyle. For several weeks following surgery, you won’t be allowed to lift anything over 10 pounds. Restrictions may last anywhere from six weeks to three months depending on the complexity of your case and how strenuous your typical daily activities are.
Q. Will I need physical therapy?
A. Prior to your surgery, your physician will determine if you can benefit from physical therapy. Physical therapy is not necessary for every patient. Typically, people who have larger, more complex hernias have a greater disruption to their abdominal wall. These patients will benefit from physical therapy. People struggling with physical function from their hernia usually use their back or hips because these are load-bearing areas of the body when your abdomen is not working properly. Physical therapy will help strengthen these areas. Because physical therapy is not always covered by insurance, ideally your physician will help you establish criteria known as a “functional deficit.”
Dr. Chike Chukwumah is director of the Hernia Center at Hartford Hospital.
Want to learn more about hernias and what surgery entails? Join us for a free community education session on Tuesday, May 29, at 6:30 p.m., at Blue Back Square in West Hartford. This session will be led by general surgeon Edward Hannoush, MD. To register, call 1.855.HHC.HERE (1.855.442.4373).