“Take two aspirin and call me in the morning” may be the punchline to an old joke, but for many years it was also the remedy most people chose when they had a headache.
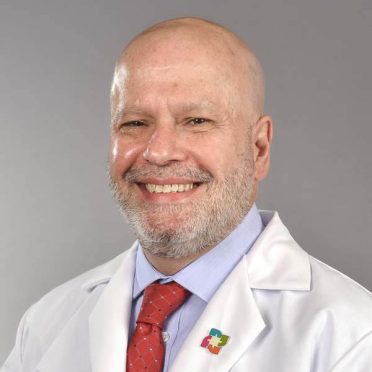
Of course, science and medicine evolve. Pain management in general and headaches in particular have become specialities within the medical profession. Dr. Joseph Casaly, a neurologist at the Mystic HealthCenter and part of the Hartford HealthCare Ayer Neuroscience Institute, has devoted the last 29 years of his career to the evaluation and management of patients experiencing headache disorders.
Here are five things to know about migraine, with comments by Dr. Casaly:
1. If you have recurrent moderate to severe headaches, you likely have migraine.
Migraines have been traditionally underrecognized as a major cause of intermittent, prominent headaches. Many patients come into my office thinking that sinus problems, allergies or neck problems are the cause of their headaches. After taking a careful history of their headache experience, however, I make a diagnosis of migraine for the vast majority of these individuals.
Researchers have created a simple questionnaire called “ID Migraine” that can be used with confidence to determine if an individual has this problem:
- Has a headache limited your activity for a day or more in the last three months?
- Are you nauseated when you have a headache?
- Does light bother you when you have a headache?
If the answer is “yes” to at least two of the three questions, there is a 93 percent probability that the responder has migraine.
2. Migraine is not a symptom, it’s a disease process caused by brain dysfunction.
I often have patients say to me, “I want to get to the bottom of what’s causing my migraines!” My answer is that they have migraines — because they have migraine. Migraine is a disease process caused by an individual having an underlying tendency to develop spontaneous pain generation in the pain pathways of the brain that supply head, face and neck structures.
This spontaneous pain signal generation is often associated with abnormal activation of other brain centers that cause associated symptoms like nausea, light and sound sensitivity, dizziness and concentration problems. To make it simpler – migraine is caused by a patient having an overly “excitable brain.” This tendency is often genetic—in fact 75 percent of patients experiencing migraine have a family history of such.
3. Migraine is one of the most disabling medical problems in the world.
The 2017 “Global Burden of Disease” study assessed “years lived with disability” of the world’s population and found headache disorders to be listed second by respondents, behind only low back pain. Migraine was the cause of 86 percent of the headache disorders.
Surprising? At first blush, yes, as we can easily think of other illnesses or injuries that are more devastating to an individual than recurrent migraine attacks. But consider that migraine affects a large percentage of the population (12 percent of all Americans) and it can burden the affected individual for many years, and sometimes nearly a lifetime, it’s easier to appreciate its impact on individuals and society in general.
4. Medication use can be “too much of a good thing.”
I often have patients say, “I used to be able to deal with my headaches by using over-the-counter painkillers, but now the headaches are getting more frequent, and worse in intensity, and they’re not working well anymore. I now have headaches almost every day, and the painkillers just take the edge off of the pain.”
When I hear this, I suspect that they have a complicating factor to their headache disorder called “medication overuse headache.” This can occur by use of simple painkillers like ibuprofen or acetaminophen at least half of all days, or combination painkillers (for example, aspirin/acetaminophen/caffeine combinations) 10 days per month or more.
Frequent painkiller use can actually dampen the brain’s own ability to regulate pain, which can lead to a vicious cycle of a patient trying to eliminate pain by increasing use of painkillers that are actually contributing to the problem. Expert medical guidance can often help reverse the situation.
5. “Frequent headaches are just something I’m going to have to learn to live with.”
Yes and no. There is no cure for migraine, and there will not be one in the foreseeable future. The tendency for one’s brain to produce migraine attacks is often hereditary and simply the way a patient’s brain works. In the headache field, we often compare it to diseases like asthma or diabetes, which cannot be eliminated from a patient by modern medicine.
On the other hand, migraine, like asthma and diabetes, can be well managed. We have effective preventive strategies that can lessen the frequency, severity and associated disability of migraine attacks. We also have ways to cut short migraine attacks, stopping them before they progress to a severe level of pain. We have a wide range of strategies, both medicinal and non-medicinal.
Finally, research into the causes and treatments for migraine is ongoing and has led to the availability of some exciting new treatments that have improved the lives of many migraine sufferers.
Dr. Joseph Casaly has office hours in the Mystic HealthCenter, 100 Perkins Farm Drive, Monday-Friday from 8 am to 4:30 pm. Call 860.889.9035 to schedule an appointment.
For more information on the Hartford HealthCare Headache Center, click here.
Not feeling well? Call your healthcare provider for guidance and try to avoid going directly to an emergency department or urgent care center, as this could increase the chances of the disease spreading.
Click here to schedule a virtual visit with a Hartford HealthCare-GoHealth Urgent Care provider.
Stay with Hartford HealthCare for everything you need to know about the coronavirus threat. Click here for information updated daily.
Stay fit. Stay happy. Stay healthy. And keep on top of COVID-19 with Hartford HealthCare’s daily text alerts. Subscribe by texting MoreLife to 31996.